Introduction: Sinusoidal obstruction syndrome (SOS) is a potentially life-threatening complication of hematopoietic stem cell transplantation (HSCT). As the immediate initiation of SOS treatment has been shown to be associated with a better prognosis, SOS prediction is clinically important. Biomarkers composed of some routine parameters, such as the aspartate aminotransferase to platelet ratio index (APRI), fibrosis-4 index (FIB-4), and albumin-bilirubin (ALBI), have been widely used to evaluate various hepatic diseases. However, the contribution of these hepatic biomarkers to the prediction and diagnosis of SOS has not been estimated yet. Here, we investigated whether routinely calculable biomarkers, endothelial activation and stress index (EASIX), APRI, FIB-4, ALBI, model for end-stage liver disease (MELD), and MELDNa were associated with the development of SOS.
Patients and Methods: A total of 141 patients (corresponding to 161 transplant cases) who underwent allogeneic HSCT at our institution between January 2012 and December 2022 were retrospectively analyzed. The median age at transplantation was 52 years (range: 19-69). The primary diseases included AML (n = 59), ALL/LBL (n = 34), MDS (n = 20), malignant lymphoma (n = 15), plasma cell neoplasm (n = 4), CML/MPN (n = 10), bone marrow failure (n = 3), and others (n = 16). The graft sources were from 30 related and 131 unrelated donors. The numbers of bone marrow, peripheral blood, and cord blood sources were 65, 29, and 67, respectively. Conditioning consisted of myeloablative (n = 68) and reduced-intensity (n = 93) regimens. Haplo-identical transplantation was not performed in this cohort. SOS was diagnosed according to the European Society for Blood and Marrow Transplantation diagnostic criteria 2023. The baseline value of each biomarker before conditioning was compared between the SOS-developing and non-SOS groups, using the Kruskal-Wallis test and a post-hoc test with the Bonferroni method. To evaluate the contribution of biomarkers on SOS diagnosis, we configured matched paired controls from non-SOS cases (three non-SOS controls per SOS case), adjusting for age, sex, last follow-up day, HLA mismatch, and hematopoietic cell transplantation-specific comorbidity index. The values of biomarkers in the SOS and matched paired control groups were compared using the Mann-Whitney U test. In the present study, the negative sign of ALBI was reversed for convenience in analysis.
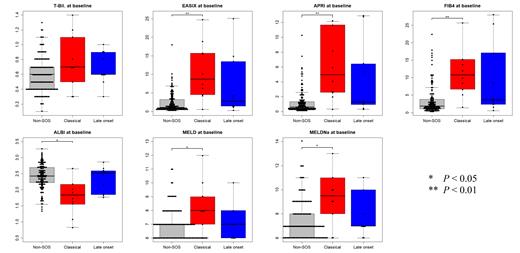
Results and Discussion: Twenty cases were diagnosed to have developed clinical SOS (10 classical SOS and 10 late onset SOS cases). All biomarkers at baseline were significantly different for classical SOS versus non-SOS cases. The median values of EASIX, APRI, FIB-4, ALBI, MELD, and MELDNa were 8.70 vs 1.09 (range: 0.57-24.68 vs 0.22-34.10, P < 0.001), 4.97 vs 0.60 (range: 0.33-32.07 vs 0.11-10.30, P < 0.001), 10.80 vs 1.84 (range: 1.37-38.01 vs 0.31-44.69, P < 0.001), 1.84 vs 2.43 (range: 0.83-3.71 vs 1.33-3.27, P = 0.012), 8.0 vs 7.0 (range: 6-12 vs 6-17, P = 0.028), and 9.5 vs 7.0 (range: 6-18 vs 6-17, P = 0.025), respectively. Moreover, among SOS cases, biomarkers at SOS diagnosis were significantly different compared with those of matched paired controls. The median values were 33.67 vs 3.90 (range: 4.54-252.18 vs 0.28-87.22, P < 0.001), 9.90 vs 1.79 (range: 3.33-127.33 vs 0.19-23.94, P < 0.001), 43.00 vs 6.80 (range: 7.91-182.27 vs 0.60-54.92, P < 0.001), 1.06 vs 2.02 (range: 0.37-1.88 vs 0.52-3.19, P < 0.001), 14.0 vs 7.0 (range: 10-30 vs 6-23, P < 0.001), and 16.5 vs 8.5 (range: 10-31 vs 6-29, P < 0.001), respectively. These results indicate that these biomarkers are associated with SOS, as well as support its diagnosis. As these biomarkers were concise, rapidly calculable, and dispensable with special techniques, their use might be clinically superior to other tests.
Conclusion: These routinely calculable biomarkers are associated with the development of SOS. Furthermore, these biomarkers are clinically useful for diagnosis of SOS. Further studies are required to improve the performance and discover an optimal biomarker.
Disclosures
Yakushijin:Astrazeneca: Honoraria; Janssen Pharmaceutical: Honoraria; Novartis: Honoraria; Asahi Kasei Pharma: Honoraria; Otsuka Pharmaceutical: Honoraria; Pfizer: Honoraria; Jazz Pharmaceuticals: Honoraria; Nippon Shinyaku: Honoraria; Chugai Pharmaceutical: Research Funding. Kitao:Nippon Shinyaku: Honoraria; Otsuka Pharmaceutical: Honoraria. Saito:Bristol Myers Squibb: Research Funding. Murayama:Otsuka Pharmaceutical Co., Ltd.: Honoraria; Novartis Pharma K.K.: Honoraria; Takeda Pharmaceutical Company Limited: Honoraria; SymBio Pharmaceuticals Limited: Honoraria; Kyowa Kirin Co.,Ltd.: Honoraria; Ono Pharmaceutical CO. Ltd..: Honoraria; Nippon Shinyaku Co., Ltd: Honoraria; Mundipharma K.K.: Honoraria; Eisai Co., Ltd.: Honoraria; Janssen Pharmaceutical K.K.: Honoraria; Bristol Myers Squibb K. K.: Honoraria; AbbVie GK: Honoraria; Chugai Pharmaceutical Co.Ltd: Honoraria. Matsuoka:Otsuka Pharmaceutical: Honoraria; Nippon Shinyaku: Honoraria; Pfizer: Honoraria. Minami:Chugai Pharmaceutical: Research Funding; Bristol Myers Squibb: Research Funding; Asahi Kasei Pharma: Research Funding; Nippon Shinyaku: Research Funding; Otsuka Pharmaceutical: Research Funding; Novartis Pharma: Research Funding; Ono Pharmaceutical: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal